This solution is powered by the same technology that powered our AI Agents CAM, DAN, and ARIA. We have combined the advanced AI technology behind our AI Agents with a first-of-its-kind orchestration layer that optimizes how AI and human experts work together. This new architecture allows us to train on millions of real RCM transactions and handle every edge case with human-in-the-loop oversight—so automations continuously learn and improve.
The result is the first fully managed RCM transformation, where AI runs the processes and brings in human experts only when needed. The outcome is a more accurate, more comprehensive solution that goes live in a fraction of the time—now strengthened by deeper industry knowledge and expert human judgment.
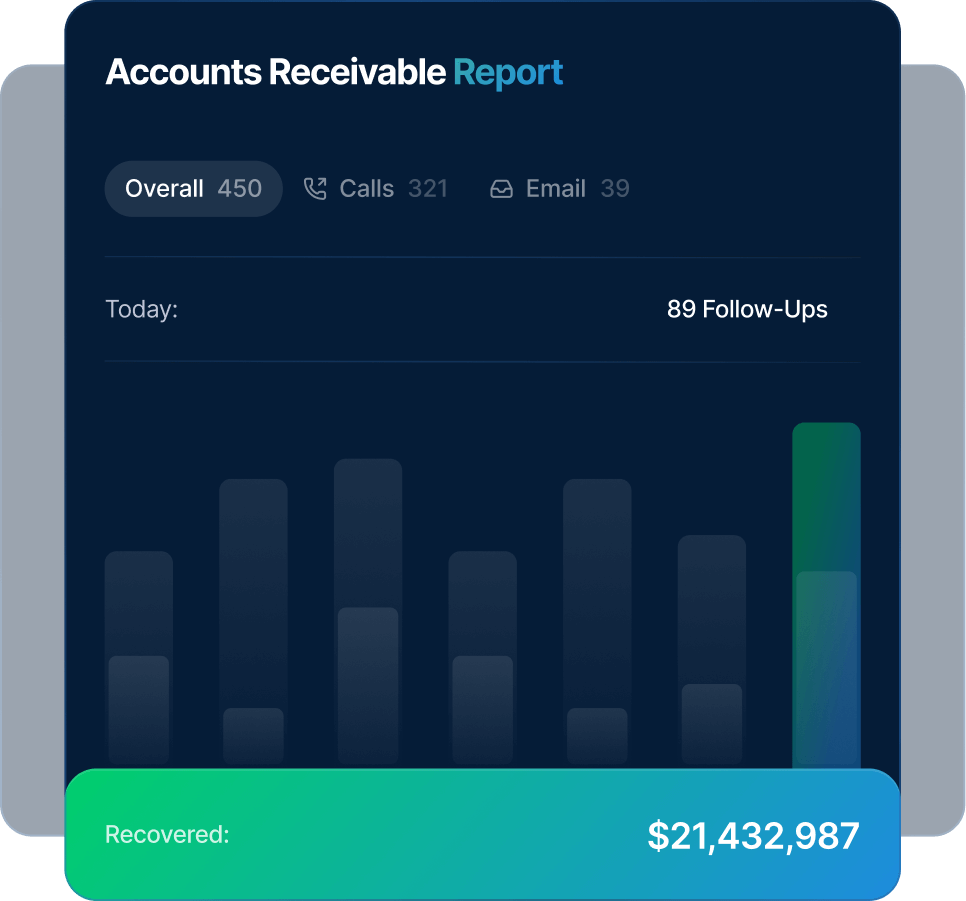
Accounts Receivable Follow-up Automated Intelligently
AI manages claim follow-ups, status checks, and prioritization automatically—while experts handle complex denials and payer exceptions to accelerate recovery and improve cash flow.
40%
Faster collections
10x
More follow-ups per FTE
20%
Better recovery on aged accounts
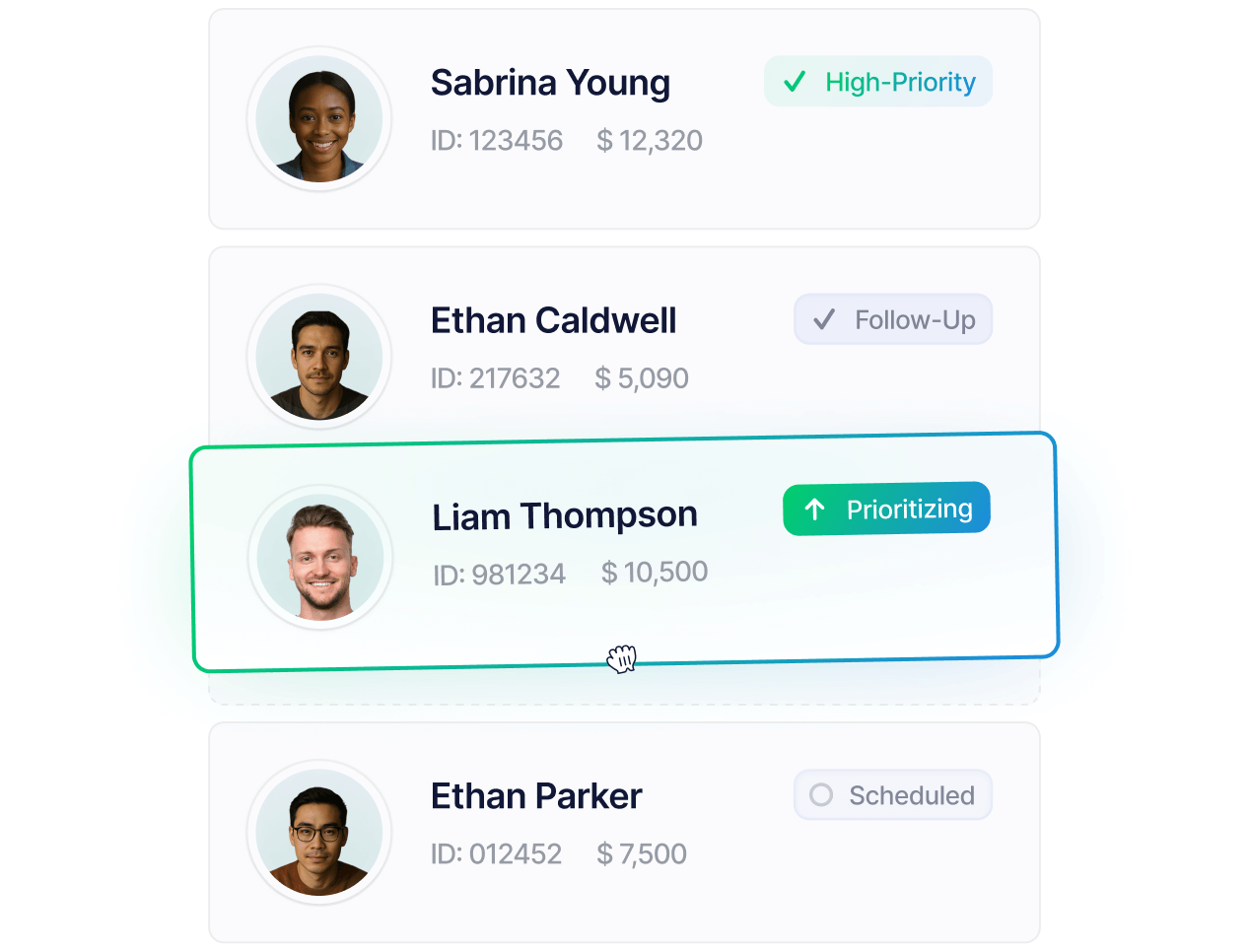
Intelligent Account Prioritization
Stop chasing the wrong accounts first
AI continuously scores and prioritizes receivables based on payer reliability, aging, and payment probability. High-value or time-sensitive accounts are surfaced instantly, while automation manages routine follow-ups in the background. Experts step in only where human strategy or payer negotiation adds value—ensuring every account gets the right level of attention.
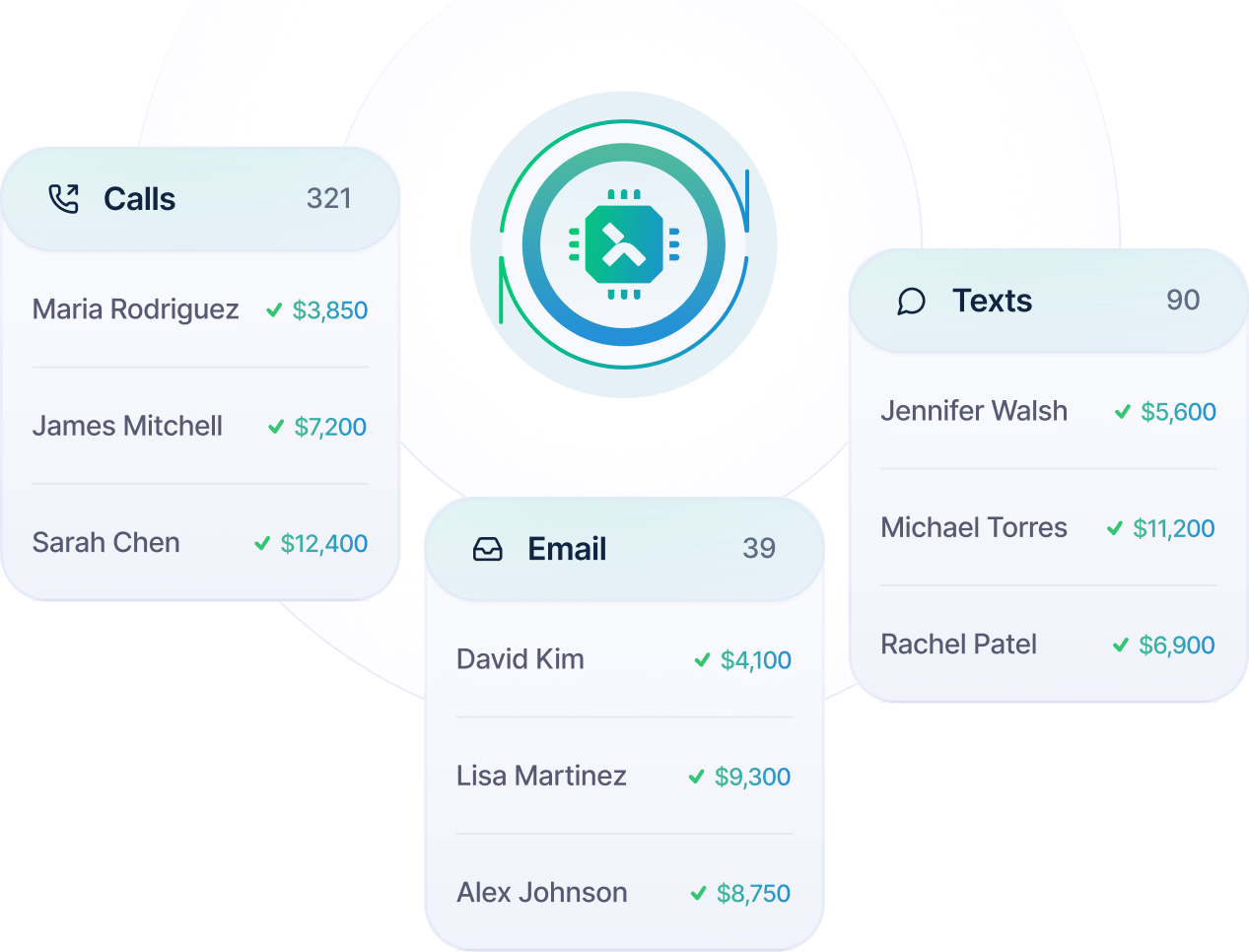
Automated Multi-Channel Follow-up
Scale Follow-Ups Without Scaling Headcount
Follow-ups happen automatically across every channel—payer portals, calls, emails, and messages—while the system records each touchpoint as it happens. If an account needs a personal touch, experienced collectors take over, using the AI’s real-time insights to resolve exceptions quickly and close balances faster.
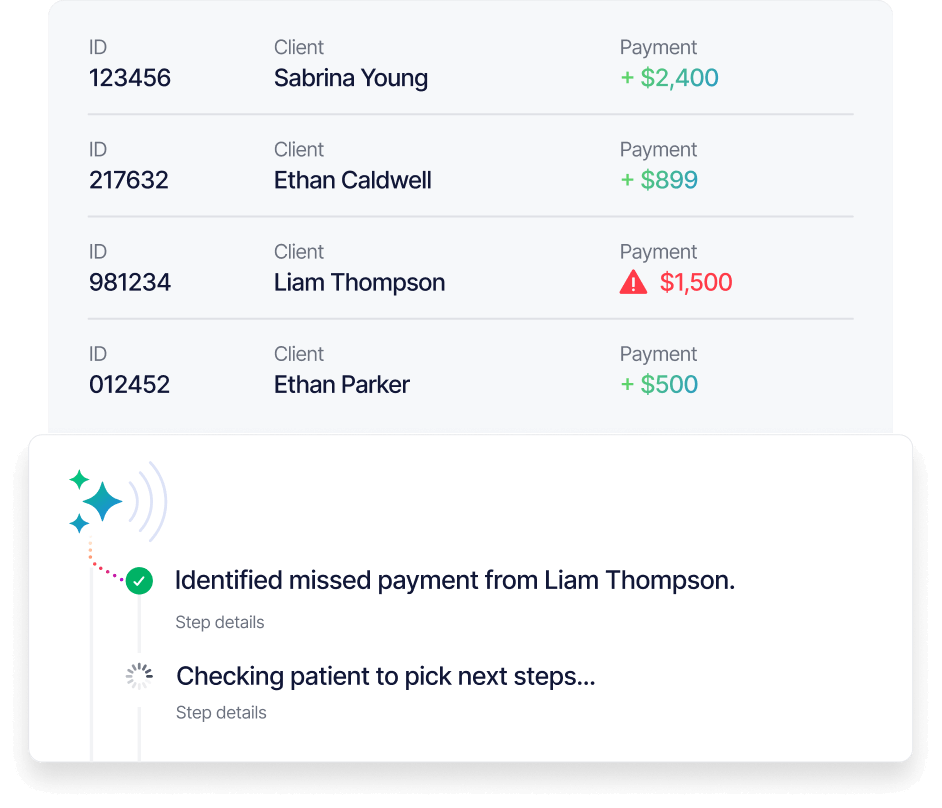
Predictive Payment Intelligence
Recover More Before Accounts Fall Behind
Predictive analytics flag accounts showing early signs of delay or denial. The system alerts your team before a problem grows, routing those cases to specialists for proactive outreach. AI guides each next step with data-backed recommendations—so action happens early, efficiently, and with confidence.

Powered by




As Featured In



