
Revenue Cycle Management
Transform Your Revenue Cycle with AI Agents
Cut operational costs and accelerate cash flow with an integrated team of AI Agents that automate your entire revenue cycle.
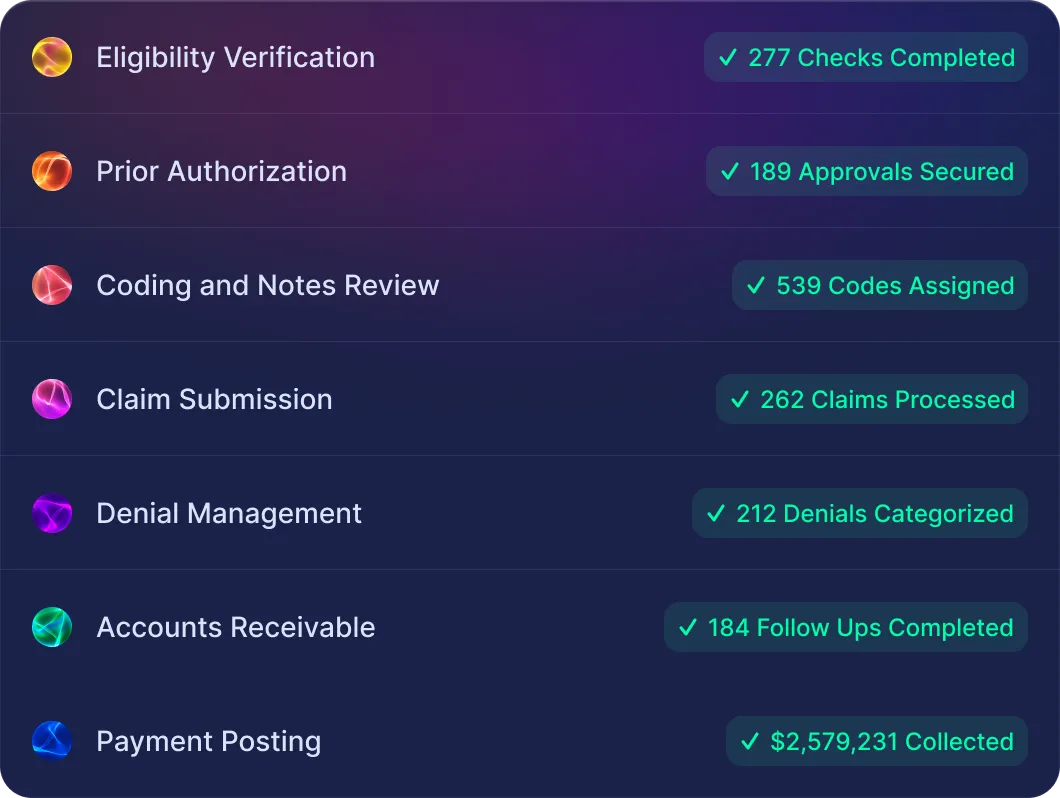








Our AI Agents automate RCM departments from start to finish, handling everything from eligibility verification to claim processing and payment posting.
Prevent Denials and Secure Coverage Upfront
Capture accurate patient data upfront to eliminate errors and rework. Slash preventable denials by up to 75% with automated eligibility checks. Seamless verification and scheduling support clean claims, boosting cash flow and reducing staff burnout.

Submit Clean Claims Quickly
Achieve 98% claim accuracy with AI Agents handling coding, notes review, and claim scrubbing. With embedded charge capture, document every billable service and conduct timely compliance audits. This proactive approach prevents undercharging and protects revenue.

Recover Revenue And Accelerate Cash Flow
Recover revenue faster with AI Agents managing denials and posting payments. Resolve disputes using AI analytics to track underpayments and boost collections. Close the loop with real-time A/R insights and payer performance metrics, capturing every dollar you've earned.





