This solution is powered by the same technology that powered our AI Agent PHIL. We have combined the advanced AI technology behind our AI Agents with a first-of-its-kind orchestration layer that optimizes how AI and human experts work together. This new architecture allows us to train on millions of real RCM transactions and handle every edge case with human-in-the-loop oversight—so automations continuously learn and improve.
The result is the first fully managed RCM transformation, where AI runs the processes and brings in human experts only when needed. The outcome is a more accurate, more comprehensive solution that goes live in a fraction of the time—now strengthened by deeper industry knowledge and expert human judgment.
Automate Every Step of Payment Posting
AI automation posts all revenue with precision and speed—reconciling payments, matching EOBs, and flagging exceptions for quick resolution.
95%
Reduced manual effort in payment posting
10x
Payments posted per agent
%20(1).svg)
Payment Posting
Streamlined, Error-Free Payment Posting
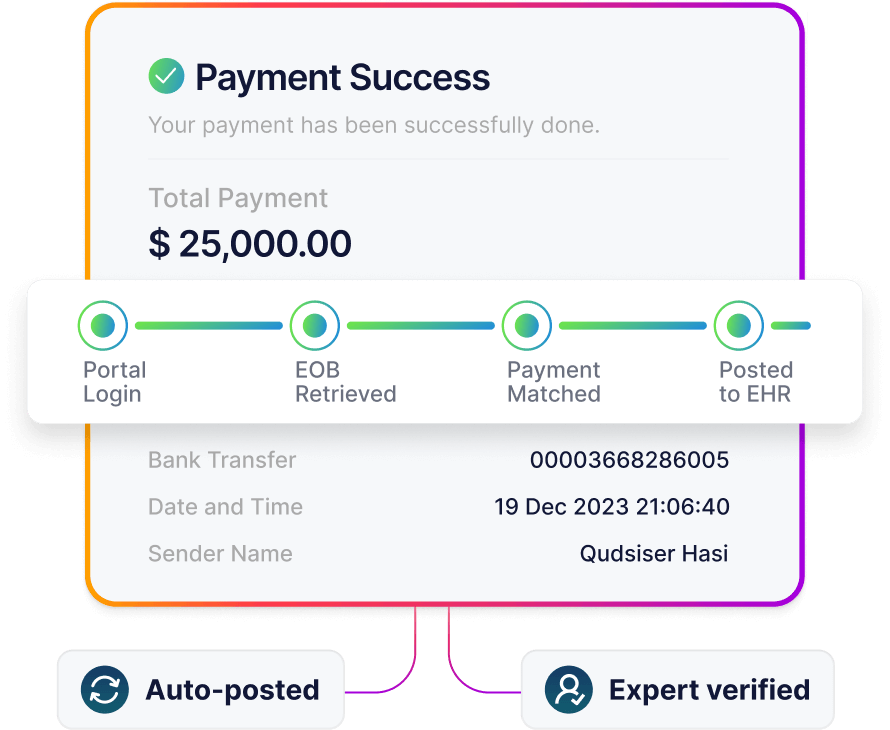
The system automates the entire posting process—from pulling remittance data to applying payments directly within your EHR. It logs into payer portals, reads EOBs, matches payments to claims, and posts them automatically. When exceptions or mismatches occur, experts handle the resolution immediately, ensuring no delay in reconciliation or reporting.
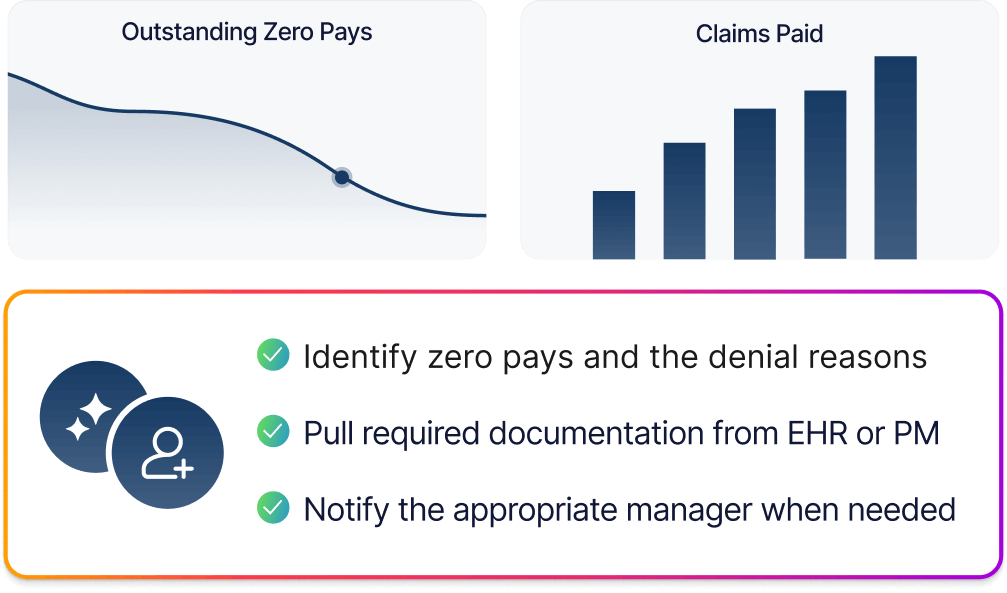
Identify Zero Pay and Patient Responsibility
Your first line of defense for all denials.
AI identifies zero pays and denial reasons, pulling documentation from your EHR or PM to prepare resubmissions automatically. If an issue requires a call, signature, or manual appeal, our experts are alerted right away to resolve it the same day.

Powered by




As Featured In



